Healing Trauma Through the Body and Brain: How Art Therapy and EMDR Help
How Trauma is Stored in the Brain and Body
When we go through something traumatic, the brain’s alarm system (the amygdala) takes over. It stores the experience as sensory fragments—images, sounds, smells, and body sensations—rather than as a clear story.
The thinking parts of the brain—like the prefrontal cortex—may shut down, and the memory doesn’t get fully processed. This is why trauma often feels like it’s happening “now,” even years later.
Neuroscientist and child trauma expert Dr. Bruce Perry explains that trauma can leave the body stuck in survival mode—ready to fight, flee, or freeze.
The Polyvagal Theory: A Key to Understanding Trauma
Dr. Stephen Porges’ Polyvagal Theory helps explain how trauma affects the body’s automatic responses. It describes three main states of the nervous system:
– Ventral vagal (safe, social, connected)
– Sympathetic (fight or flight)
– Dorsal vagal (shut down, freeze)
When we feel safe, we’re in the ventral vagal state—able to connect, think clearly, and be creative. But trauma can push us into survival states (fight/flight/freeze), where we feel numb, anxious, or disconnected.
Art Therapy: Working With the Body Through the Senses
Art therapy helps people express what can’t be put into words. When someone draws, paints, or sculpts their feelings or body sensations, they’re tapping into the sensory part of the brain—right where trauma lives.
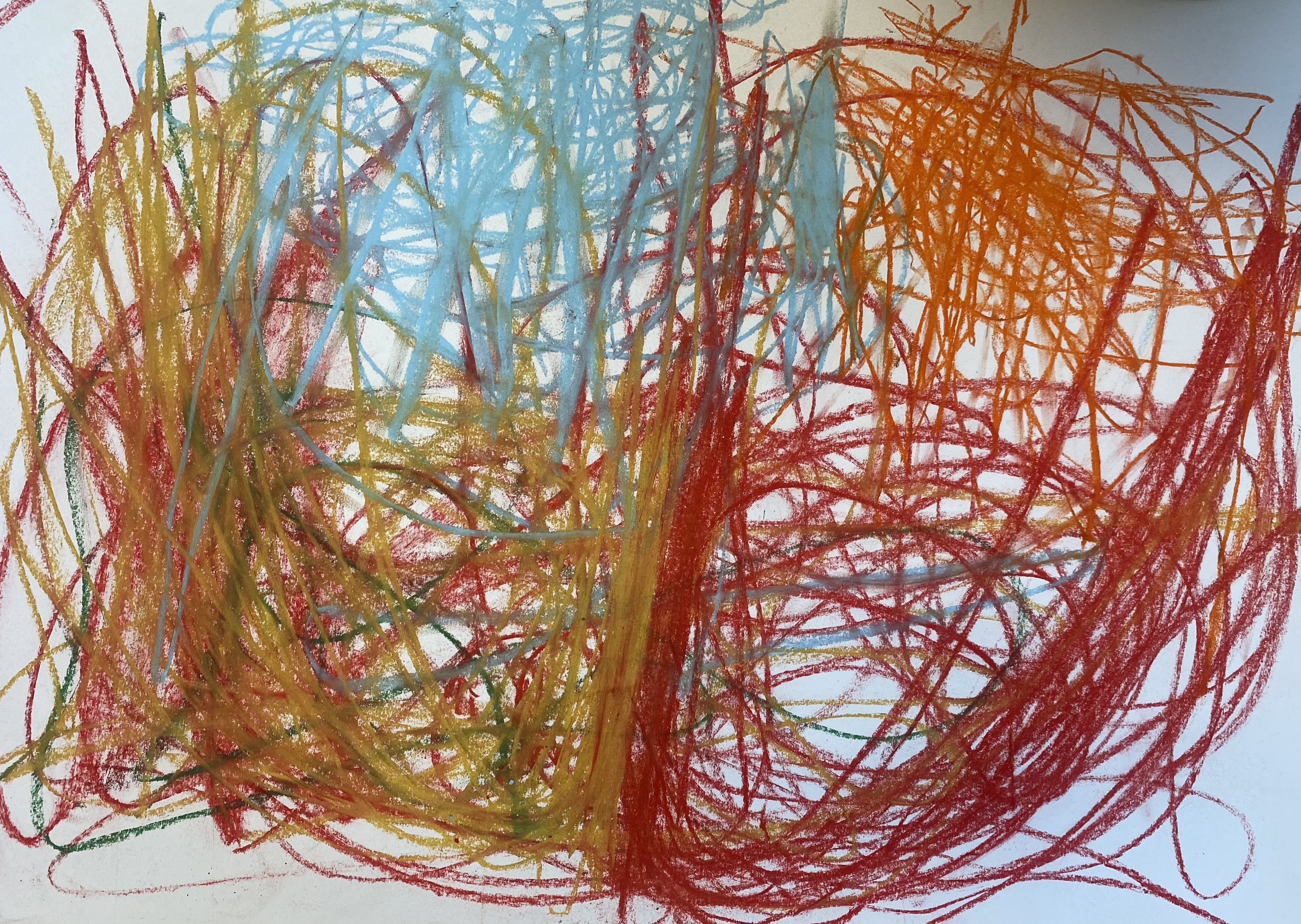
Polyvagal-informed art therapy focuses on safety, rhythm, and sensory experiences to help regulate the nervous system. Examples include:
– Using soothing materials (like soft pastels or warm clay)
– Creating repetitive marks or movements (which can calm the system)
– Exploring body maps to gently identify where sensations are felt
– Working in quiet, low-stimulation environments
These interventions help activate the ventral vagal state, where healing can begin.
EMDR: Bilateral Stimulation to Help the Brain Process
EMDR, developed by Francine Shapiro, uses bilateral stimulation—like eye movements, tapping, or tones alternating left and right—to help the brain reprocess traumatic memories.
This works by activating both sides of the brain, which helps connect the emotional and logical parts. Research indicates that EMDR can reduce physical stress reactions and help individuals recall difficult events without feeling overwhelmed.
According to Shapiro’s Adaptive Information Processing model, trauma gets “stuck” in the brain. EMDR helps it move and settle into a more peaceful, integrated memory.
Why the Body Matters: A Whole-Person Approach
Both art therapy and EMDR go beyond talk. They work with the body, senses, and nervous system—essential when trauma is stored as sensations rather than words.
Together, they help people:
– Feel safer in their bodies
– Reconnect with emotions and sensations
– Make sense of past experiences
– Build resilience and calm
Putting It All Together in Therapy
A trauma-informed therapist may:
1. Start with safety—using gentle art or grounding to stabilize the nervous system
2. Use art materials to help access emotions or memories through the body
3. Introduce EMDR to reprocess traumatic memories with bilateral stimulation
4. Pay attention to body cues, breathing, and regulation throughout
5. Use Polyvagal-informed techniques like rhythm, co-regulation, and safe social connection
References & Resources
– Perry, B. D. (2006). The Neurosequential Model of Therapeutics. https://childtrauma.org
– Shapiro, F. (2001). EMDR: Basic Principles, Protocols, and Procedures. https://www.emdria.org
– Porges, S. (2011). The Polyvagal Theory
– Elbrecht, C. (2018). Healing Trauma with Guided Drawing
– https://www.polyvagalinstitute.org
– https://www.sensorimotorarttherapy.com